Over the last two decades, the number of health research institutions has increased with many focusing on health policy and systems research (HPSR). However, locally generated research is not used consistently in health-related decisions in low- and middle-income countries, particularly in sub-Saharan Africa. What is more, little is known about what makes it more or less likely that evidence will play a role in policy-making, nor about the profile of health systems research institutions operating in different contexts.
To support these efforts, the Alliance and the Doris Duke Charitable Foundation commissioned three studies to explore the evidence-to-policy process in Ethiopia, Ghana and Mozambique. We worked with Jimma University in Ethiopia, the Regional Institute for Population Studies in Ghana, and Instituto Nacional de Saúde in Mozambique to undertake surveys and in-depth interviews with representatives from 54 locally based research institutions and 41 health policy-makers, the studies explored the entire chain of evidence generation – from conception of the research idea, through to its synthesis and dissemination. The national teams coordinated with a research group at the International Health Policy Program in Thailand to ensure a common approach and research protocols.
Four briefs were developed to summarize key findings, one from each country along with a cross-cutting brief and have been published today. The studies found that:
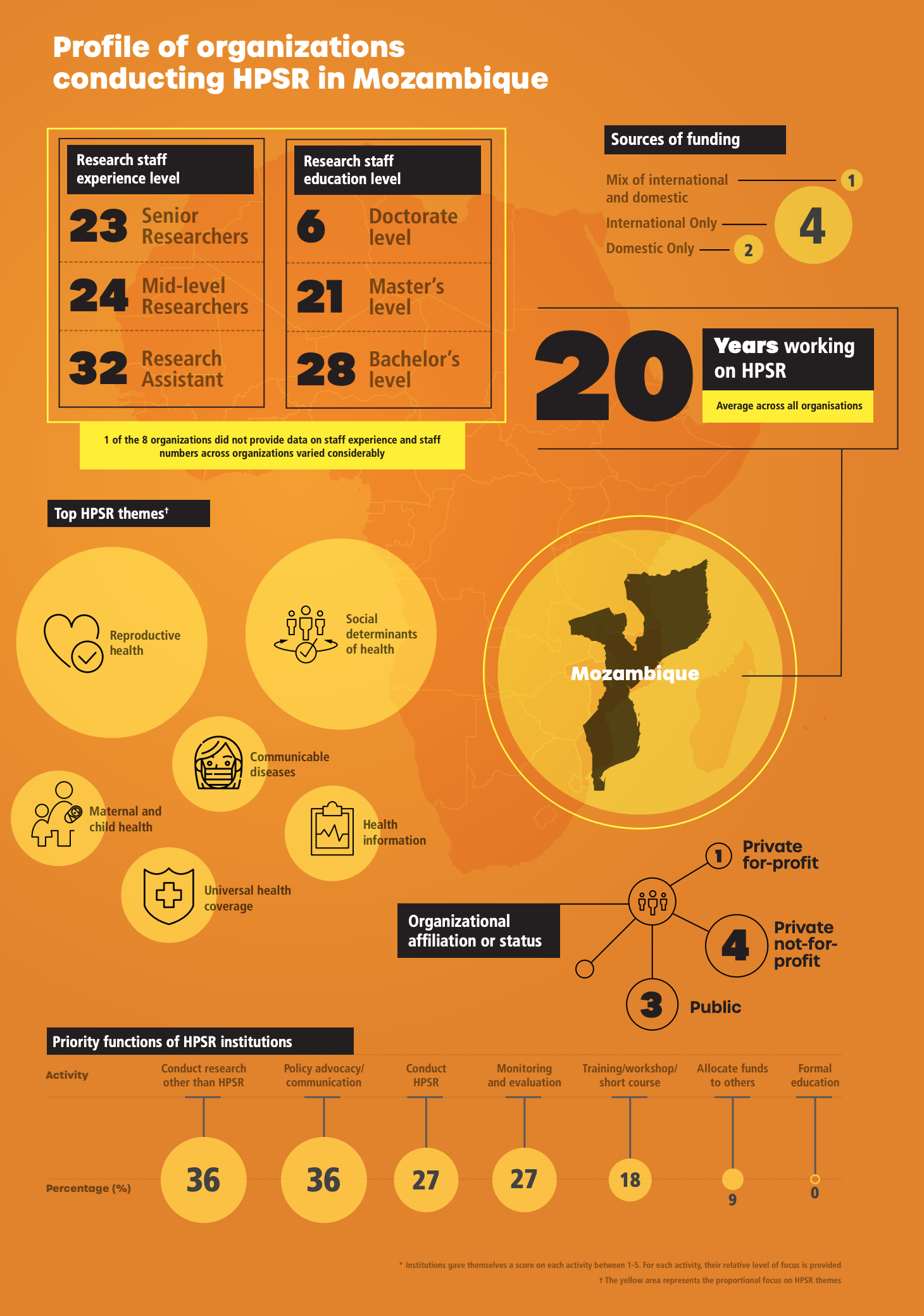
- Health systems research in these countries is conducted by a mix of public and private not-for-profit entities, and that the number of for-profit research firms is low. This includes health units embedded in – or officially linked to – national ministries of health, specialist faculties housed in universities, professional associations, and private not-for-profit research firms.
- In all three countries, the distribution of research skills is uneven, but recruitment and retention dynamics play out and affect research institutions differently. A significant number of staff, especially senior researchers, are concentrated in just one or two public institutions, which has an impact on the capacity of some organizations.
- Developing HPSR studies is not the main area of focus for research institutions in Ethiopia and Mozambique who put more emphasis on training and advocacy activities, along with conducting general health research. Ghana is more focused in this respect with over 90% of institutions engaged in HPSR evidence generation.
- Funding is a major constraint for all research institutions. Across all three settings, little core funding for HSPR was reported, which prevents research organizations from improving their overall research processes through investments at the institutional level according to respondents.
The country-level briefs profile the institutions in greater detail. They all provide a graphic overview of the institutions, their areas of focus, their researchers and their links with policy-makers. The figure below is an example overview from Mozambique.
The briefs also offer reflections on key gaps and areas of opportunity, providing recommendations that could be useful for research institutions, national governments and funders.
